See Explanation
[]
Hematology
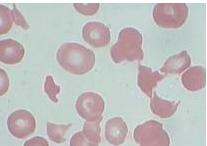
hemolytic anemia
hemolytic uremic syndrome
A 32-year-old woman presents to an urgent care clinic with a 5-day history of worsening fatigue, dark urine, and diffuse abdominal discomfort, which started after a diarrheal illness characterized by severe, bloody stools. She reports decreased urine output over the past 24 hours. Her medical history is otherwise unremarkable. On examination, she appears pale and jaundiced. Vital signs reveal a blood pressure of 90/55 mm Hg, pulse rate of 115/min, respiratory rate of 18/min, and temperature of 37.2 °C. Abdominal palpation elicits diffuse tenderness but no guarding or rebound. Petechiae are noted on her lower extremities. The rest of her physical examination is non-contributory. Laboratory findings are now available: The peripheral blood smear shows schistocytes and scant platelets without clumps. The direct antiglobulin (Coombs) test is negative. Given her presentation, what is the most likely diagnosis and the appropriate immediate management strategy?
| Lab Parameter | Value | Reference Range |
|---|---|---|
| Haptoglobin | Undetectable | 0.3-2.0 g/L |
| Hemoglobin | 61 g/L | 125-170 g/L |
| Leukocyte count | 6.8 x 10^9/L | 3.5-10.5 x 10^9/L |
| Platelet count | 37 x 10^9/L | 130-380 x 10^9/L |
| Reticulocytes | 9.8% | 0.5-1.5% |
| Creatinine | 318 µmol/L | 70-120 µmol/L |
| Blood Urea Nitrogen (BUN) | 25 mmol/L | 2.5-7.5 mmol/L |
| Potassium | 5.8 mmol/L | 3.5-5.0 mmol/L |
| Urinalysis Blood | 3+ | |
| Urinalysis Protein | 3+ | |
| Urinalysis Microscopic examination | several granular casts |
Edit question